MRCP revision battle 25.1: Neuroleptic malignant syndrome
MRCP revision battle 25.2: Behcets disease
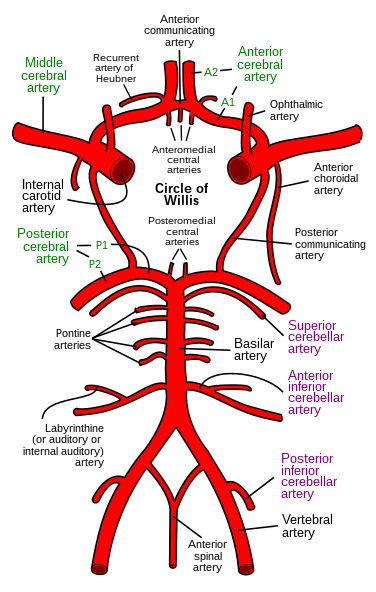
MRCP revision battle 25.3: Subarachnoid haemorrhage
MRCP revision battle 25.4: Normal pressure hydrocephalus
MRCP revision battle 25.5: Gas gangrene
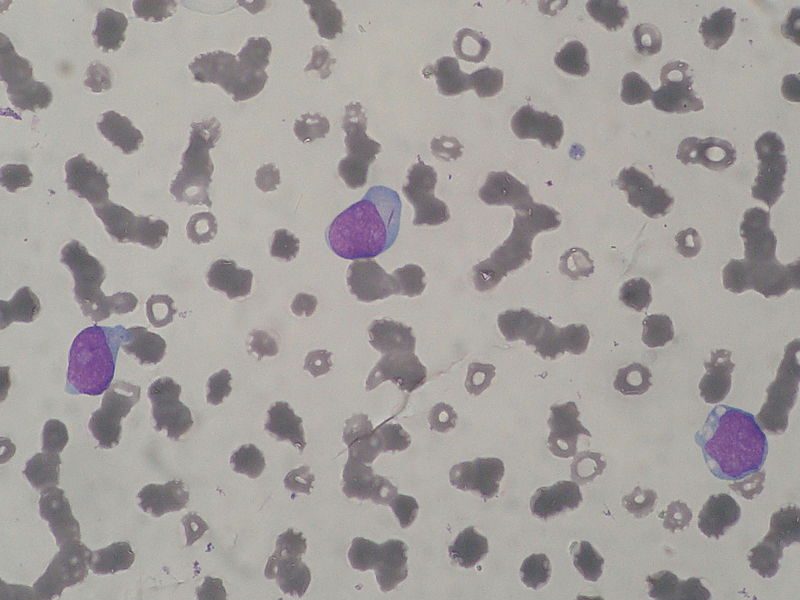
MRCP revision battle 25.6: Methaemoglobinaemia
MRCP revision battle 25.7: The weeverfish
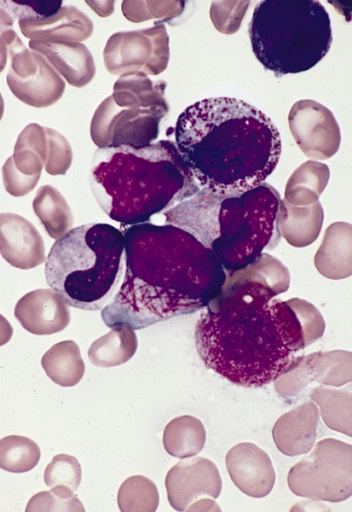
MRCP revision battle 25.1: Neuroleptic malignant syndrome
A nice straightfoward battle to begin with...
Neuroleptic malignant syndrome is a life-threatening condition associated with use of antipsychotic drugs.
Symptoms and signs include:
- hyperthermia
- rigidity/muscle cramps
- extrapyramidal signs
- autonomic dysfunction (labile BP, sweating, urinary incontinence
- confusion
Investigations show:
- raised CK
- raised WCC
Treatment is:
- cooling
- dantrolene (a muscle relaxant; note dantrolene is also used in malignant hyperthermia, which will be one of tomorrows battles)
Now on to a slightly less straightforward battle, Behcets disease...