Aortic dissection is a scary condition with a mortality rate of 1% per hour. But before we jump into it, lets begin with a quick recap of some basic anatomy.
The layers of the aorta are, from inside out:
- tunica intima = epithelial cells
- tunica media = smooth muscle and elastic fibres
- tunica adventitia = connective tissue
Aortic dissection usually involves blood collecting in the media.
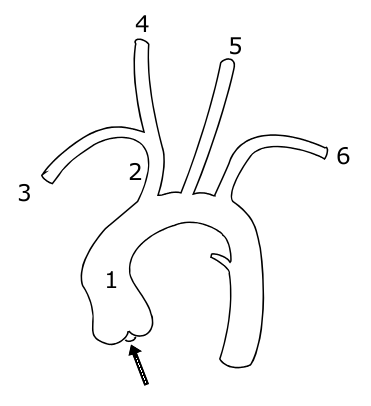
The aorta itself leaves the heart, goes up into an arch and then down again, giving off branches as it goes. The picture below shows the vessels coming off the aorta:
1 indicates the ascending aorta, 2 the brachiocephalic trunk, 3 the right subclavian artery, 4 the right common carotid, 4 the right common carotid, 5 the left common carotid and 6 the left subclavian artery.
A knowledge of this anatomy aides understanding of the signs and symptoms of aortic dissection.
So what are the features of an aortic dissection?
- sudden onset of 'tearing' or 'ripping' pain
- if pain intrascapular, likely a descending dissection
- MI
- stroke
- parathesia of arms
- hemiparesis
- many others, depending on the part of the aorta affected
Signs to look out for include:
- aortic regurgitation - present in 1/3 ascending dissections
- pulse deficit in an arm - present in 15%
- BP difference in arms >20mmHg (but note 'normal' individuals may have a BP difference)
Aortic dissections may be classified using either the Stanford or DeBakey systems:
- Stanford A = ascending dissection - accounts for 2/3 of dissections
- this covers DeBakey I - ascending and descending aorta involved and
- DeBakey II - ascending aorta only involved
- Stanford B = descending aorta only dissected (distal to left subclavian artery) - accounts for 1/3 of dissections
Management of aortic dissection:
- if type A - IV labetalol and urgent surgery
- if type B - IV labetalol only
Complications associated with type A dissections include:
- aortic regurgitation
- inferior MI
- pericardial effusion
- carotid dissection
- loss of pulses
Investigations for dissection:
- CXR
- shows widened mediastinum in 70% of cases
- Ring sign - calcification of aorta with wall displaced >5mm
- CT
- TOE
Risk factors for dissection include:
- hypertension (80%)
- Marfans
- Noonans
- Turners
- trauma
- pregnancy
- coarctation
- congenital bicuspid valve
- giant cell artertitis
- cocaine use
If you feel motivated to read more, I'd recommend this webpage: http://www.aorticdissection.com/Aortic%20Diagnosis.htm
A 'war' for yesterday's questions is
here