So the carrot is dangled, and here are the sticks:
MRCP revision battle 27.1: Heparin induced thrombocytopenia (HIT)
MRCP revision battle 27.2: Sarcoidosis
MRCP revision battle 27.3: Lofgren's syndrome
MRCP revision battle 27.4: Pancreatitis
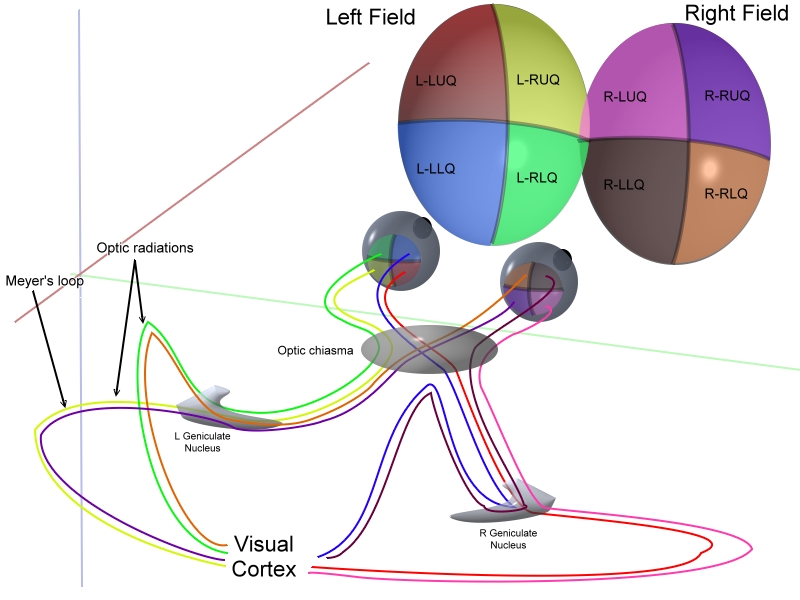
MRCP revision battle 27.5: Visual field defects
MRCP revision battle 27.6: Paroxysmal nocturnal haemoglobinuria
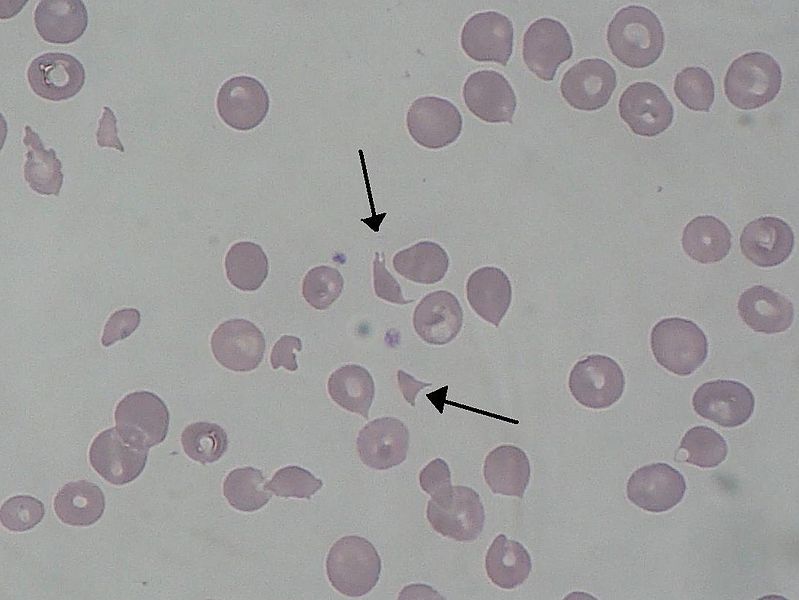
MRCP revision battle 27.7: Poikilocytosis
MRCP revision battle 27.1: Heparin induced thrombocytopenia (HIT)
Heparin induced thrombocytopenia is one of those fabulous conditions whose name explains it all: low platelets, caused by heparin. It is often abbreviated to HIT, which confused me greatly when I first had a patient affected by it and my consultant declared "ah, he's got HIT" which made me wonder who he was suspecting of abuse on the ward...
Technically there are 2 types of HIT:
- Type 1 - occurs in first 2 days, is non-immune and the platelet count spontaneously recovers
- Type 2 - occurs 4 to 10 days after starting heparin, is immune-mediated and potentially life-threatening.
However, when HIT is mentioned, people generally mean type 2.
HIT is caused by antibodies against the heparin-platelet factor 4 complex. These antibodies can be found in 90% of patients with HIT... but may also be present in unaffected patients taking heparin.
Ironically, although HIT is characterised by low platelets it is an incredibly pro-thrombotic condition. As a result patients are likely to get PEs/DVTs and warfarin must absolutely not be started (since warfarin is initially prothrombotic too). As you can see HIT causes something of a management problem - thrombosis due to the treatment you would give for thrombosis...
Management of HIT will involve specialist haematological input but in terms of MRCP question answers think:
- stop heparin
- stop/reverse warfarin
- give lepirudin (=highly specific direct inhibitor of thrombin)
Note that HIT is more likely with unfractionated than LMW heparin.
Onwards to sarcoidosis...