So today's battles are:
MRCP revision battle 24.1: Primary biliary cirrhosis
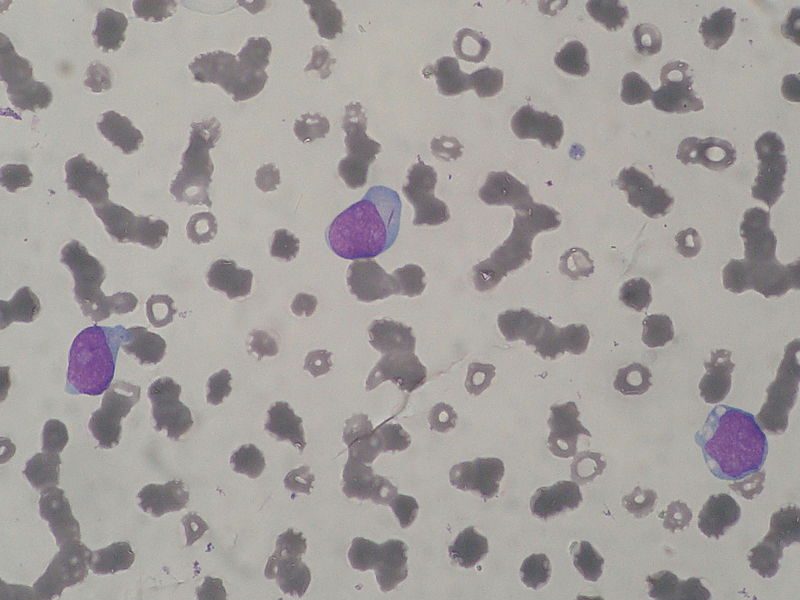
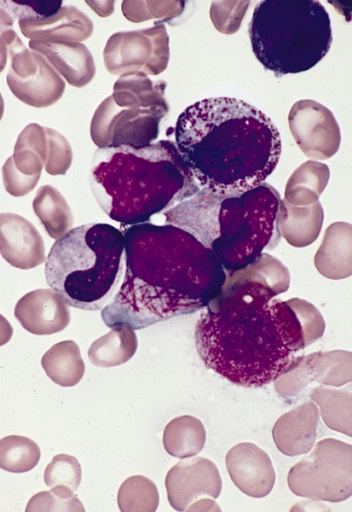
MRCP revision battle 24.2: Acute Myeloid Leukaemia
MRCP revision battle 24.3: Acute Promyelocytic Leukaemia
MRCP revision battle 24.4: Angioid retinal streaks
MRCP revision battle 24.5: SIADH
MRCP revision battle 24.6: Hyponatraemia
MRCP revision battle 24.7: Neutropenia and neutrophillia
MRCP revision battle 24.1: Primary biliary cirrhosis
I've never bonded well with this topic so this battle is a personal Waterloo for me...
Primary biliary cirrhosis is thought to be an autoimmune condition in which the interlobular bile ducts are damanged by chronic granulomatous inflammation.
The result of this is:
- progressive cholestasis
- cirrhosis
- portal hypertension
Females are more affected than males (9:1) and it tends to present in middle age.
It is associated with many other autoimmune conditions, including sjogrens, RA, systemic sclerosis, thyroid disease...
Primary biliary cirrhosis is often found incidentally by a raised alk phos on LFTs.Initially other LFTs may be normal but as the disease progresses bilirubin rises and PT may increase.
Associated signs (in late disease) include:
- jaundice
- xanthelasma
- hepatosplenomegaly
- clubbing
Complications include:
- osteoporosis
- portal hypertension
- variceal haemorrhage
Diagnosis includes antibodies:
- AMA M2 is highly specific and is positive in 98% of cases
- SMA is positive in 30%
- raised IgM
Treatment is:
- cholestyramine for itching
- osteoporosis prophylaxis
- transplant
Once jaundice develops, without transplant the survival is < 2yrs.
On to AML...