Today is another 'octopus' day with 8 battles to embrace (three of which are mercifully brief)
So the topics are:
MRCP revision battle 18.1: Warfarin
MRCP revision battle 18.2: Psoriasis
MRCP revision battle 18.3: Beau's lines
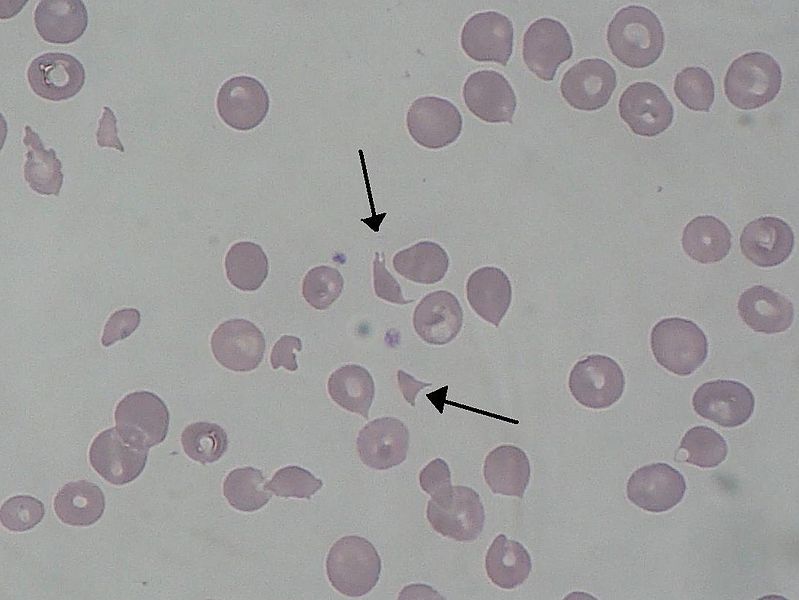
MRCP revision battle 18.4: Elliptocytosis
MRCP revision battle 18.5: Aortic stenosis
MRCP revision battle 18.6: Polymyalgia rheumatica
MRCP revision battle 18.7: Threadworm
MRCP revision battle 18.8: Pseudohypoparathyroidism
MRCP revision battle 18.1: Warfarin
Ah, warfarin... everyone's favourite out-of-hours bleep as a houseofficer. Originally made as a rat poison, it quickly became a favourite in the UK for the treatment of DVTs, PEs and prevention of clots associated with mechanical heart valves.
Warfarin works by
inhibiting vitamin K epoxide reductase, which prevents vitamin K being recycled. Since vitamin K is a cofactor for factors
II, VII, IX and X it decreases coagulation.
Note however that vitamin K is also a cofactor for protein C and protein S, which help inhibit the clotting cascade. As protein C is initially affected more than the clotting factors by lack of vitamin K
warfarin is initially a procoagulant and when started therefore increases the risk of thrombosis.
Warfarin is monitored by INR. The targets are:
- PE/DVT: INR 2-3
- metallic valve: INR 3-4
The duration of anticoagulation depends on the cause of the clot:
- below knee DVT after surgery: 6 weeks
- above knee DVT/PE after surgery: 3 months
- DVT/PE without precipitating factor identified: 6 months
1-2% of patients on warfarin have a haemorrhage per year.
Other complications of warfarin treatment include:
- increased risk of osteoporosis
- purple toe syndrome - toes turn purple ?secondary to cholesterol deposits 3 to 8 weeks after starting warfarin
Warfarin levels are notoriously difficult to regulate.
Things which increase the effect of warfarin include:
- erythromycine/clarithromycin
- metronidazole
- hyperthyroidism
- cranberry juice
- alcohol
- amiodarone
- propranolol
- fluconazole
- isoniazod
- cimetidine
- omeprazole
Things which decrease the effect of warfarin include:
- rifampacin
- carbamazepine
- chlordiazepoxide
- avocado in excess!
Management of INR outside the desired range depends both on the level and if there is bleeding:
- major bleed
- stop warfarin
- give vit K 5-10mg IV
- give prothrombin complex (II, VII, IX, X) or FFP if this is not available
- INR>8 but no/minimal bleeding
- stop warfarin
- give vit K 2.5-5mg PO/0.5-1mg IV
- restart warfarin when INR<5
- INR 5-8, no bleeding
- stop warfarin
- restart when INR<5
- INR 5-8 minor bleeding
- stop warfarin
- give 1-2.5mg vitamin K PO
- restart when INR<5
As an aside, with an eye on the future, a new drug called
dabigatran is looking to usurp warfarin as king of the anticoagulants. Trials such as
RELY and
RECOVER have shown dabigatran to be non-inferior to warfarin in preventing thrombosis, to cause fewer bleeding adverse effects and even better not require regular blood tests to check levels. Of course its expensive and so not yet approved...
On to the second battle of the day,
psoriasis...